Outcomes of external and endonasal dacryocystorhinostomy according to a modified Lacrimal Symptom Questionnaire (Lac-Q)
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 12 No. 2 (2023),
31 December 2023
,
Page 55-61
https://doi.org/10.51329/mehdiophthal1470
Abstract
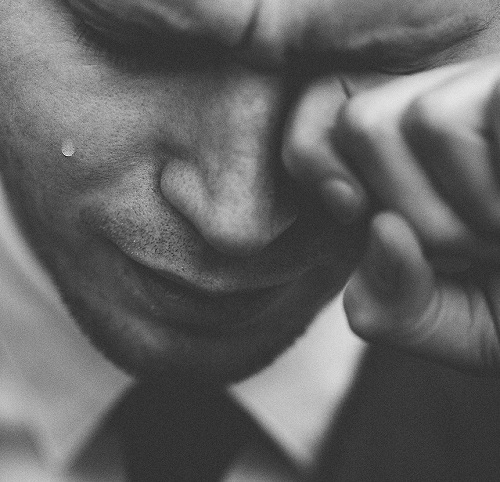
Background: Nasolacrimal duct obstruction is usually treated using endoscopic or external dacryocystorhinostomy (DCR). The anatomic outcomes of both the endoscopic and external approaches are considered excellent. However, anatomic success does not translate into patient satisfaction. The current study assessed pre- and postoperative lacrimal problems using the symptom-based Lacrimal Symptom Questionnaire (Lac-Q) and investigated patient satisfaction depending on the choice of surgical technique.Methods: A total of 112 eligible patients with lacrimal problems treated using external or endonasal DCR at the ophthalmology and ear, nose, and throat clinics at Skane University Hospital, Sweden, over a four-year period, were enrolled in this retrospective study. Patients were considered eligible if they experienced preoperative epiphora and had lacrimal duct stenosis. They were offered treatment using either external or endonasal DCR and were allowed to freely choose the technique. Exclusion criteria consisted of previous ipsilateral DCR, congenital NLDO, age < 18 years, presence of cancer, previous orbital trauma, or noncompliance with postoperative follow-up. After surgery, the patients were sent the Lac-Q to evaluate their lacrimal symptoms pre- and postoperatively. Complementary questions were added pertaining to the operative scar and the patients’ overall satisfaction with the operation.
Results: In total, 67 (60%) patients with ages ranging from 18 to 88 years completed the questionnaire, 33 (49%) of whom underwent external DCR and 34 (51%) endonasal DCR. Of the 67 respondents, 51 (76%) were women and 16 (24%) were men. Patients scored preoperative lacrimal problems highly on the Lac-Q, reporting both symptomatic and social problems due to epiphora. Following surgery, the group that underwent external DCR remained home from work for 2 – 14 days (median, 3.5 days). However, 17 (52%) were retired. After the endonasal DCR, the patients remained home for 0 – 7 days (median, 2 days). Most patients were satisfied after DCR surgery, with both techniques significantly improving total, lacrimal symptom, and social impact scores (all P < 0.001). No differences in postoperative satisfaction were observed between the external DCR and endonasal DCR groups (P > 0.05). A small number of patients expressed scar-related concerns after external DCR.
Conclusions: The patients perceived lacrimal problems as a significant symptomatic and social burden. Postoperative satisfaction and symptom relief were good regardless of the surgical approach. Further prospective studies assessing patient satisfaction and its correlation with anatomical and functional success rates after external and endonasal DCR could provide robust, practical, real-world implications.
- Abstract Viewed: 0 times
- Full Text PDF Downloaded: 0 times


