Clinical anatomy: cornea and ocular surface
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 14 No. 3 (2025),
27 September 2025
,
Page 60-72
https://doi.org/10.51329/mehdiophthal1524
Abstract
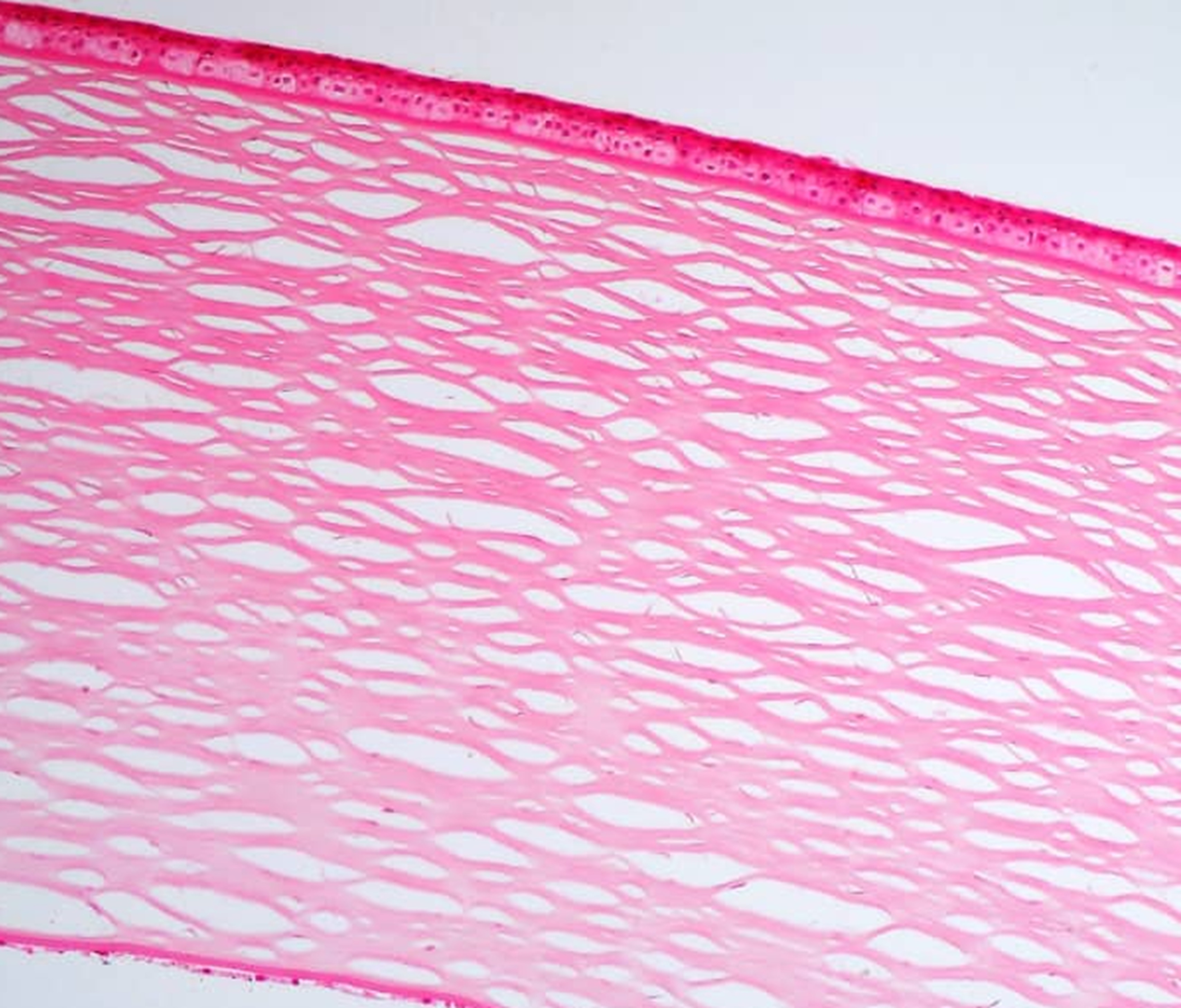
Background: The cornea and ocular surface serve as a vital barrier and the eye’s primary refractive medium, requiring precise coordination to maintain transparency, structural integrity, and immune protection. Constantly exposed to environmental stressors, this interface relies on the stability of the tear film, epithelial architecture, mucin layers, and limbal stem cells to preserve function. Disruption in any component can impair vision and increase vulnerability to disease. Advances in imaging and molecular diagnostics have deepened our understanding of these structures, offering new avenues for early detection and personalized treatment strategies. A comprehensive review is needed to integrate recent findings and assess their clinical relevance.Methods: A targeted literature search was conducted using PubMed/MEDLINE and Google Scholar to identify English-language publications from 1 January 2000 to 30 May 2025. Keywords included “anatomy,” “histology,” “cornea,” “ocular surface,” “epithelium,” “Bowman’s layer,” “stroma,” “Descemet’s membrane,” “endothelium,” “conjunctiva,” “lacrimal functional unit,” and “eyelids.” Studies were selected irrespective of design, and reference lists of included articles were manually screened for additional relevant sources.
Results: Eighty-six publications were reviewed. Findings highlight that the cornea and ocular surface constitute an integrated anatomical and physiological continuum essential for optical clarity, visual acuity, and ocular health. This dynamic unit comprises the cornea, conjunctiva, tear film (mucin, aqueous, and lipid layers), meibomian glands, goblet cells, and the limbal stem cell niche. Collectively, these elements provide lubrication, immune defense, epithelial homeostasis, and structural integrity. Disruption in any component—such as in dry eye disease, limbal stem cell deficiency, or meibomian gland dysfunction—can precipitate epithelial breakdown, neovascularization, or stromal scarring, ultimately compromising vision. Recognizing this interdependence has reframed ocular surface disease as a multifactorial condition rather than an isolated disorder. A comprehensive understanding of the structural and immunological dynamics of this system is therefore critical for refining surgical strategies and developing targeted therapies.
Conclusions: The cornea and ocular surface components function synergistically to maintain a transparent, stable refractive surface essential for vision. Their coordinated roles in protection, lubrication, immune defense, and tissue repair reveal the importance of anatomical understanding for developing targeted therapies and improving clinical outcomes. A comprehensive understanding of this anatomy is essential for clinicians and researchers aiming to develop more precise therapeutic strategies and surgical techniques to enhance patient outcomes and preserve visual function. Future research should focus on advancing regenerative strategies and personalized treatments to address complex ocular surface disorders more effectively.
- Abstract Viewed: 0 times
- Full Text PDF Downloaded: 0 times


