Bilateral superior oblique suture extension in pediatric A-pattern esotropia
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 14 No. 3 (2025),
27 September 2025
,
Page 163-170
https://doi.org/10.51329/mehdiophthal1529
Abstract
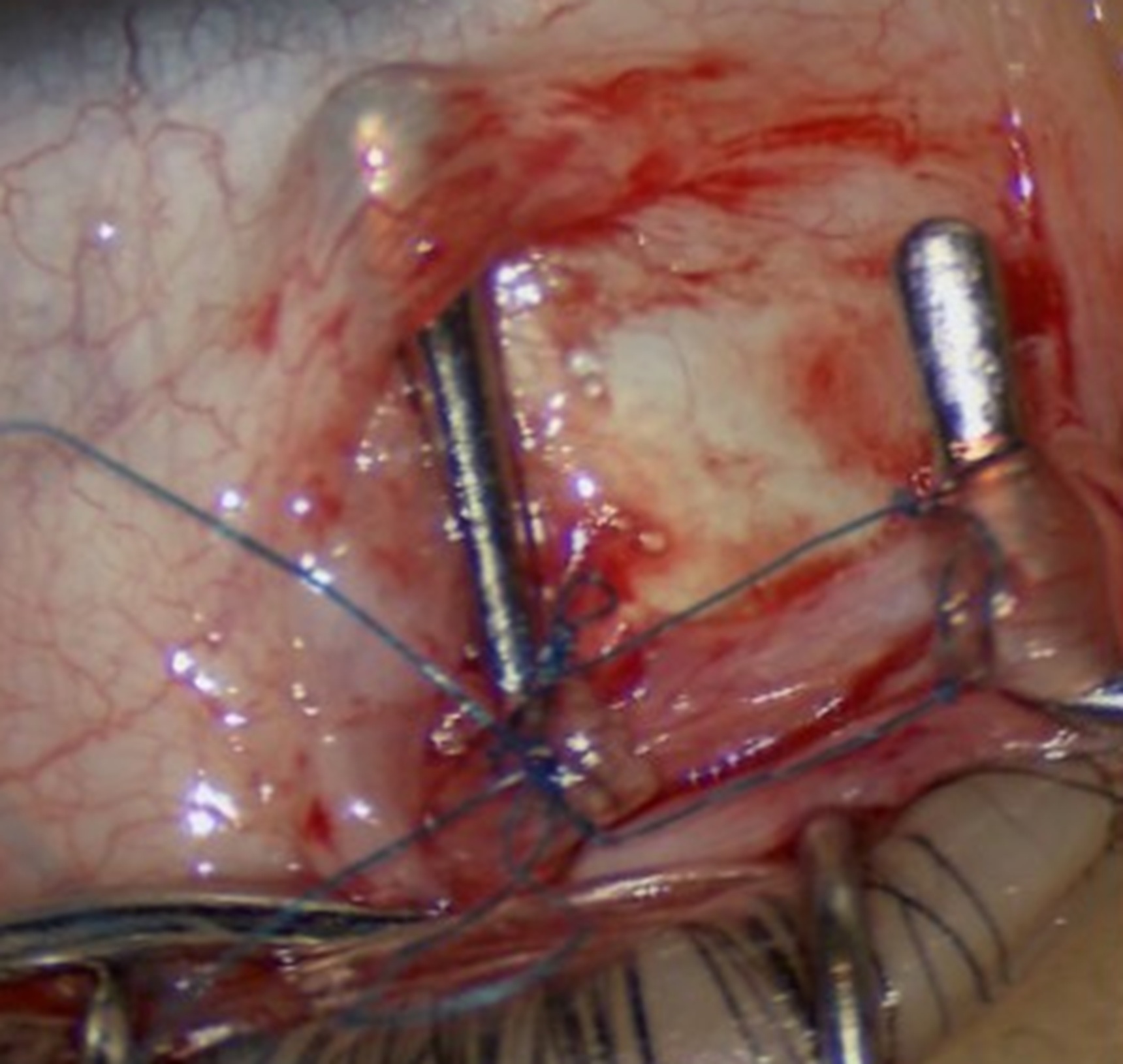
Background: A-pattern esotropia is defined as an increase of more than 10 prism diopters (PD) divergence in down-gaze than in up-gaze. The long-term outcomes of bilateral superior oblique tendon suture extension (SOSE), a hardware-free technique, were evaluated in pediatric A-pattern esotropia with bilateral superior oblique overaction (bi-SOOA), addressing complications associated with traditional silicone spacers and tenotomy.Methods: In this retrospective cohort study, all participants with A-pattern esotropia and bi-SOOA underwent bilateral SOSE using nonabsorbable polypropylene sutures combined with medial rectus recession. Preoperative and postoperative assessments included prism cover testing in nine gazes, fundus photography for objective torsion quantification, and grading of superior oblique overaction (SOOA).
Results: This study included 64 eyes from 32 children with a mean (SD) age of 7.0 (3.1) years and a mean (SD) postoperative follow-up of 35.2 (15.6) months (range: 8–55). The mean (SD) A-pattern esodeviation collapsed from 23.4 (7.7) PD preoperatively to 2.4 (2.3) PD postoperatively (P < 0.001), representing an 88.3% reduction. The mean (SD) horizontal esodeviation improved from 37.5 (10.9) PD to 1.7 (1.8) PD in primary gaze (P < 0.001). The mean (SD) objective fundus torsion decreased from 10.9 (2.5) degrees to 1.1 (1.4) degrees (P < 0.001), with no cases of torsional diplopia or vertical deviation. SOOA grades normalized from 2.8 (0.7) to 0.2 (0.4) (P < 0.001). No suture-related complications were observed, and alignment stability was maintained through to the final follow-up visit.
Conclusions: In pediatric A-pattern esodeviation surgery, SOSE provided biomechanical precision, anatomical preservation, and elimination of hardware-related risks. Its effectiveness in collapsing A-pattern esotropia, normalizing torsion, and achieving durable outcomes establishes it as a first-line surgical intervention for bi-SOOA. This study addresses a significant gap in pediatric ophthalmology, offering extended follow-up data and highlighting the value of minimally invasive, growth-compatible techniques in protecting visual development. Larger randomized trials with extended follow-up are needed to confirm the efficacy and safety of this procedure for A-pattern esotropia.
- Abstract Viewed: 0 times
- Full Text PDF Downloaded: 0 times


