Higher-order aberrations following wavefront-guided photorefractive keratectomy and laser in situ keratomileusis
Medical hypothesis, discovery & innovation in optometry,
Vol. 1 No. 2 (2020),
31 October 2020
,
Page 100-104
https://doi.org/10.51329/mehdioptometry112
Abstract
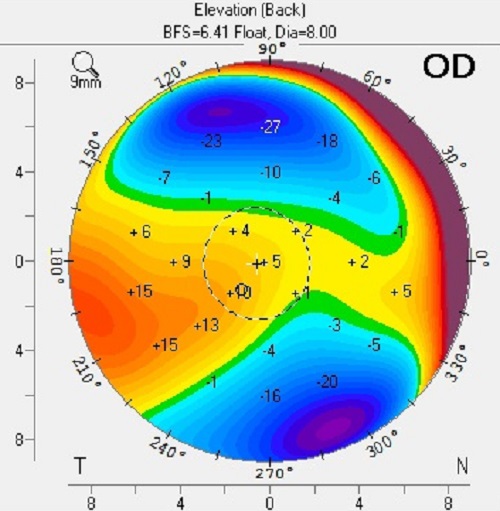
Background: We aimed to evaluate higher-order aberrations (HOAs) following wavefront-guided photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK) in patients with myopia and myopic astigmatism.Methods: This retrospective observational case-control study included patients who underwent wavefront-guided PRK (40 eyes of 20 patients) or LASIK (40 eyes of 20 patients) between August 2018 and November 2018 at the refractive surgery unit of Kayseri City Hospital Eye Clinic, Turkey. The corrected distance visual acuity (CDVA), manifest refraction, corneal topography, and HOAs were evaluated preoperatively and 3 months postoperatively in all patients.
Results: The mean age ± standard deviation (SD) was 27.13 ± 5.54 years and 29.10 ± 4.38 years in the PRK and LASIK groups, respectively (P = 0.06). Both groups had a mean CDVA of 1.00. The mean ± SD of spherical and spherical equivalent values was -2.09 ± 1.56 diopter (D) and -3.03 ± 1.72 D in the PRK group and -2.23 ± 1.69 D and -3.35 ± 1.71 D in the LASIK group, respectively (P = 0.58). When the preoperative and postoperative HOAs and root mean square (RMS) values (for a 6-mm pupil diameter) were compared in the PRK group, a significant difference was found in vertical coma and total RMS values (P = 0.003 and P less than 0.001, respectively); in the LASIK group, there was a significant difference in preoperative and postoperative vertical coma and total RMS values (P = 0.0.001 and P less than 0.001, respectively). There was no significant difference in preoperative and postoperative vertical coma values between the two groups (P = 0.735 and P = 0.583, respectively).
Conclusions: In terms of HOAs, total RMS values decreased significantly and vertical coma values increased significantly at 3 months postoperatively in both PRK and LASIK groups. However, there were no differences between the two groups.
Keywords:
- high-order aberrations
- HOAs
- corneal wavefront aberrations
- laser in situ keratomileusis
- photorefractive keratectomy
- LASIK
- PRK
- vertical coma
- root mean square
- RMS
- postoperative
- Abstract Viewed: 131 times
- Full Text PDF Downloaded: 0 times