Microbiological Profile of Corneal Ulcers at a Tertiary Referral Center
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 8 No. 1 (2019),
10 March 2019
,
Page 16-21
Abstract
The aim of this study was to describe patient demographics, microbiological profile, and antibiotic susceptibility of corneal ulcer at a tertiary referral center to improve and optimize diagnosis and treatment of this potentially blinding entity and to reduce antibiotic misuse. Detailed external and slit-lamp bio-microscopic examination of 123 consecutive patients with suspected corneal ulcer was performed at an ophthalmology clinic. Corneal scraping was carried out under slit-lamp bio-microscopy. The obtained material was inoculated on culture media and smeared on a slide for Gram's staining for morphological identification of bacteria and fungus. For samples that developed colony in culture media, antibiotic susceptibility testing was performed. In a significant percentage of patients (72%) neither bacterial agents nor fungi were the cause of corneal ulcer. Of the 34 culture-proven corneal ulcers, in 79% of the cases, bacteria were detected while in 21% of cases, fungi were found. Of the 27 bacterial corneal ulcers, the majority were (67%) caused by Gram-positive bacteria, of which 50% were Streptococcus pneumoniae, and in the Gram-negative bacterial corneal ulcers, most of the cases (44%) were caused by Pseudomonas aeruginosa. In the antibiotic susceptibility report, Streptococcus pneumoniae, Staphylococcus aureus, Pseudomonas aeruginosa, and Escherichia coli were resistant to Cotrimoxazole (TS), Streptococcus pneumoniae to Erythromycin (E), Staphylococcus aureus to Peniciline (PG), Pseudomonas aeruginosa to Ceftriaxone (CRO) and Nitrofurantoin (NI), and finally, Escherichia coli to Gentamicin (GM). In conclusion, in a significant number of the patients neither bacterial agents nor fungi were offending microorganisms and bacteria were the most common agent of microbiological corneal ulcer, found in 79% of culture-proven corneal ulcers, followed by fungus, found in 21% of culture-proven corneal ulcers.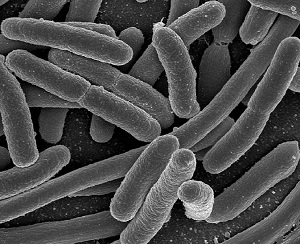
References
Whitcher JP, Srinivasan M. Corneal ulceration in the developing world--a silent epidemic. Br J Ophthalmol. 1997;81(8):622-3. doi: 10.1136/bjo.81.8.622 pmid: 9349145
Collier SA, Gronostaj MP, MacGurn AK, Cope JR, Awsumb KL, Yoder JS, et al. Estimated burden of keratitis--United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63(45):1027-30. pmid: 25393221
Green M, Apel A, Stapleton F. Risk factors and causative organisms in microbial keratitis. Cornea. 2008;27(1):22-7. doi: 10.1097/ICO.0b013e318156caf2 pmid: 18245962
Suwal S, Bhandari D, Thapa P, Shrestha MK, Amatya J. Microbiological profile of corneal ulcer cases diagnosed in a tertiary care ophthalmological institute in Nepal. BMC Ophthalmol. 2016;16(1):209. doi: 10.1186/s12886-016-0388-9 pmid: 27899093
Schaefer F, Bruttin O, Zografos L, Guex-Crosier Y. Bacterial keratitis: a prospective clinical and microbiological study. Br J Ophthalmol. 2001;85(7):842-7. pmid: 11423460
Alexandrakis G, Alfonso EC, Miller D. Shifting trends in bacterial keratitis in south Florida and emerging resistance to fluoroquinolones. Ophthalmol. 2000;107(8):1497-502. doi: 10.1016/s0161-6420(00)00179-2 pmid: 10919897
Zhang C, Liang Y, Deng S, Wang Z, Li R, Sun X. Distribution of bacterial keratitis and emerging resistance to antibiotics in China from 2001 to 2004. Clin Ophthalmol. 2008;2(3):575-9. pmid: 19668756
Ray KJ, Prajna L, Srinivasan M, Geetha M, Karpagam R, Glidden D, et al. Fluoroquinolone treatment and susceptibility of isolates from bacterial keratitis. JAMA Ophthalmol. 2013;131(3):310-3. doi: 10.1001/jamaop hthalmol.2013.1718 pmid: 23307105
Oldenburg CE, Lalitha P, Srinivasan M, Rajaraman R, Ravindran M, Mascarenhas J, et al. Emerging moxifloxacin resistance in Pseudomonas aeruginosa keratitis isolates in South India. Ophthalmic Epidemiol. 2013;20(3):155-8. doi: 10.3109/09286586.2013.7909 78 pmid: 23662986
Fintelmann RE, Hoskins EN, Lietman TM, Keenan JD, Gaynor BD, Cevallos V, et al. Topical fluoroquinolone use as a risk factor for in vitro fluoroquinolone resistance in ocular cultures. Arch Ophthalmol. 2011;129(4):399-402. doi: 10.1001/archophthalmol.2 011.45 pmid: 21482865
Murray Patrick R, Baron Eleen J. Manual of Clinical Microbiology. Virginia: ASM Press; 2007.
Lavaju P, Arya SK, Khanal B, Amatya R, Patel S. Demograhic pattern, clinical features and treatment outcome of patients with infective keratitis in the eastern region of Nepal. Nepal J Ophthalmol. 2009;1(2):101-6. pmid: 21141001
Leck AK, Thomas PA, Hagan M, Kaliamurthy J, Ackuaku E, John M, et al. Aetiology of suppurative corneal ulcers in Ghana and south India, and epidemiology of fungal keratitis. Br J Ophthalmol. 2002;86(11):1211-5. pmid: 12386069
Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Palaniappan R. Epidemiological characteristics and laboratory diagnosis of fungal keratitis. A three-year study. Indian J Ophthalmol. 2003;51(4):315-21. pmid: 14750619
Dunlop AA, Wright ED, Howlader SA, Nazrul I, Husain R, McClellan K, et al. Suppurative corneal ulceration in Bangladesh. A study of 142 cases examining the microbiological diagnosis, clinical and epidemiological features of bacterial and fungal keratitis. Aust N Z J Ophthalmol. 1994;22(2):105-10. pmid: 7917262
Tewari A, Sood N, Vegad MM, Mehta DC. Epidemiological and microbiological profile of infective keratitis in Ahmedabad. Indian J Ophthalmol. 2012;60(4):267-72. doi: 10.4103/0301-4738.98702 pmid: 22824594
Chalita MR, Hofling-Lima AL, Paranhos A, Jr., Schor P, Belfort R, Jr. Shifting trends in in vitro antibiotic susceptibilities for common ocular isolates during a period of 15 years. Am J Ophthalmol. 2004;137(1):43-51. doi: 10.1016/s0002-9394(03)00905-x pmid: 14700643
Mohammadpour M, Mohajernezhadfard Z, Khodabande A, Vahedi P. Antibiotic susceptibility patterns of pseudomonas corneal ulcers in contact lens wearers. Middle East Afr J Ophthalmol. 2011;18(3):228-31. doi: 10.4103/0974-9233.84053 pmid: 21887079
Rahimi F, Hashemian MN, Khosravi A, Moradi G, Bamdad S. Bacterial keratitis in a tertiary eye centre in Iran: a retrospective study. Middle East Afr J Ophthalmol. 2015;22(2):238-44. doi: 10.4103/0974-9233.151870 pmid: 25949085
- Abstract Viewed: 1174 times
- Full Text PDF Downloaded: 853 times


