Comparative Analysis of LASIK Flap Diameter and its Centration Using Two Different Femtosecond Lasers
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 8 No. 3 (2019),
20 September 2019
,
Page 241-249
Abstract
The aim of this study was to compare the diameter, accuracy, variability, and centration with respect to the limbus of corneal flaps created by two femtosecond lasers, the VisuMax, and Wavelight FS200, for laser in situ keratomileusis (LASIK) and how these flaps affect visual outcomes. This is a retrospective chart review of flap morphology created during LASIK Surgery. Overall, 168 eyes underwent flap creation using the WaveLight FS200 laser, and on 189 eyes, the VisuMax laser was used. Of these total number, flap morphology was analyzed in a random sample of 158 eyes; 80 with the Visumax laser and 78 with the WaveLight FS200 laser. Intraoperative photos of the flaps taken by the Wavelight Allegretto EX500 were analyzed. Flap diameters and centration were measured using Adobe Acrobat Pro. All patients had visual acuity measurements including uncorrected distance visual acuity (UDVA), corrected distance visual acuity (CDVA), spherical equivalent refraction (SE) and refractive astigmatism recorded three months postoperatively. Greater than 90% of patients in both groups achieved a UDVA of 20/20 postoperatively. The mean difference between targeted and achieved flap diameter was 0.50 +/- 0.15 mm in the VisuMax group and 0.35 +/- 0.15 millimeters (mm) in the FS200 group (P<0.01). The flap diameters of the VisuMax group were more precise with a variance of 0.024 mm compared to a variance of 0.038 mm in the FS200 group (P<0.05). VisuMax flaps were more nasally displaced (log(NA/TA) = -0.21 +/- 0.10 mm) compared to the FS200 flaps (log(NA/TA) = 0.03 +/- 0.10 mm), (P< 0.01). We concluded that both the VisuMax and FS200 created flaps larger than the preoperative targeted diameter. VisuMax created corneal flaps that had a greater degree of deviation from the targeted diameter when compared to flaps from the FS200. However, there was less variance in the VisuMax flap diameter. In addition, VisuMax flaps were more nasally displaced. There were no statistically significant differences in visual outcomes when comparing the two femtosecond lasers.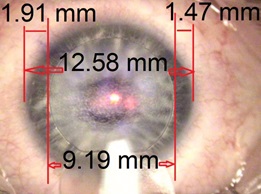
References
Sugar A, Rapuano CJ, Culbertson WW, Huang D, Varley GA, Agapitos PJ, et al. Laser in situ keratomileusis for myopia and astigmatism: safety and efficacy: a report by the American Academy of Ophthalmology. Ophthalmology. 2002; 109(1):175-87. doi: 10.1016/s0161-6420(01)00966-6 pmid: 11772601
Varley GA, Huang D, Rapuano CJ, Schallhorn S, Boxer Wachler BS, Sugar A, et al. LASIK for hyperopia, hyperopic astigmatism, and mixed astigmatism: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111(8): 1604-17. doi: 10.1016/j.ophtha.2004.05.016 pmid: 15288995
Solomon KD, Fernandez de Castro LE, Sandoval HP, Biber JM, Groat B, Neff KD, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009;116(4):691-701. doi: 10.1016/j.ophtha.2008.12.037 pmid: 19344821
Pajic B, Vastardis I, Pajic-Eggspuehler B, Gatzioufas Z, Hafezi F. Femtosecond laser versus mechanical microkeratome-assisted flap creation for LASIK: a prospective, randomized, paired-eye study. Clin Ophthalmol. 2014;8:1883-9. doi: 10.2147/OPTH.S68124 pmid: 25284975
McAlinden C. Corneal refractive surgery: past to present. Clin Exp Optom. 2012;95(4):386-98. doi: 10.1111/j. 1444-0938.2012.00761.x pmid: 22672114
Kezirian GM, Stonecipher KG. Comparison of the IntraLase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg. 2004;30 (4):804-11. doi: 10.1016/j.jcrs.2003.10.026 pmid: 15093642
Aristeidou A, Taniguchi EV, Tsatsos M, Muller R, McAlinden C, Pineda R, et al. The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis (Lond). 2015;2:12. doi: 10.1186/s40662-015-0022-6 pmid: 26605365
Zhang Y, Chen YG, Xia YJ. Comparison of corneal flap morphology using AS-OCT in LASIK with the WaveLight FS200 femtosecond laser versus a mechanical microkeratome. J Refract Surg. 2013;29(5):320-4. doi: 10.3928/1081597X-20130415-03 pmid: 23659230
Torrisi L, Roszkowska AM, Urso M, Signorino A, Aragona P, Cutroneo M. Use of the Femtosecond Lasers in Ophthalmology. EPJ Web of Conferences. 2018;167:05004. doi: 10.1051/epjconf/201816705004
Huhtala A, Pietila J, Makinen P, Uusitalo H. Femtosecond lasers for laser in situ keratomileusis: a systematic review and meta-analysis. Clin Ophthalmol. 2016; 10:393-404. doi: 10.2147/OPTH.S99394 pmid: 27022236
Salomao MQ, Wilson SE. Femtosecond laser in laser in situ keratomileusis. J Cataract Refract Surg. 2010;36(6):1024-32. doi: 10.1016/j.jcrs.2010.03.025 pmid: 20494777
Melki SA, Azar DT. LASIK complications: etiology, management, and prevention. Surv Ophthalmol. 2001;46(2):95-116. pmid: 11578645
Kanellopoulos AJ, Asimellis G. Three-dimensional LASIK flap thickness variability: topographic central, paracentral and peripheral assessment, in flaps created by a mechanical microkeratome (M2) and two different femtosecond lasers (FS60 and FS200). Clin Ophthalmol. 2013;7:675-83. doi: 10. 2147/OPTH.S40762 pmid: 23580024
Colombo-Barboza MN, Colombo-Barboza GN, Colombo-Barboza LR, Matuoka ML, Neto AL, de Freitas D. Reproducibility of laser in situ keratomileusis flap thickness using a new multifunctional femtosecond laser platform and correlation with clinical preoperative measurements. J Cataract Refract Surg. 2018;44(7):811-7. doi: 10.1016/j.jcrs.2018.05.008 pmid: 30055689
Eleftheriadis H, Prandi B, Diaz-Rato A, Morcillo M, Sabater JB. The effect of flap thickness on the visual and refractive outcome of myopic laser in situ keratomileusis. Eye (Lond). 2005;19(12):1290-6. doi: 10.1038/sj.eye.6701775 pmid: 15618975
Zheng Y, Zhou Y, Zhang J, Liu Q, Zhai C, Wang Y. Comparison of laser in situ keratomileusis flaps created by 2 femtosecond lasers. Cornea. 2015;34(3):328-33. doi: 10.1097/ ICO.0000000000000361 pmid: 25603229
Parafita-Fernandez A, Garcia-Gonzalez M, Katsanos A, Gros-Otero J, Teus M. Two Femtosecond Laser LASIK Platforms: Comparison of Evolution of Visual Acuity, Flap Thickness, and Stromal Optical Density. Cornea. 2019;38(1):98-104. doi: 10.1097/ICO.0000000000001784 pmid: 30308583
Moshirfar M, Hoggan RN, Muthappan V. Angle Kappa and its importance in refractive surgery. Oman J Ophthalmol. 2013;6(3):151-8. doi: 10.4103/0974-620X.122268 pmid: 24379548
Tsai YY, Lin JM. Ablation centration after active eye-tracker-assisted photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2000;26(1):28-34. doi: 10.1016/s0886-3350(99)00328-4 pmid: 10646143
Azar D, Koch D. LASIK : Fundamentals, Surgical Techniques, and Complications. Marcel Dekker2003.
Lee BH, McLaren JW, Erie JC, Hodge DO, Bourne WM. Reinnervation in the cornea after LASIK. Invest Ophthalmol Vis Sci. 2002;43(12):3660-4. pmid: 12454033
Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015;122(4):669-76. doi: 10. 1016/j.ophtha.2014.10.004 pmid: 25458707
Zhang YL, Liu L, Cui CX, Hu M, Li ZN, Cao LJ, et al. Comparative study of visual acuity and aberrations after intralase femtosecond LASIK: small corneal flap versus big corneal flap. Int J Ophthalmol. 2013;6(5):641-5. doi: 10.3980/ j.issn.2222-3959.2013.05.16 pmid: 24195040
- Abstract Viewed: 738 times
- Free Full Text PDF Downloaded: 690 times


