Neutrophil to Lymphocyte and Platelet to Lymphocyte Ratios in Normal Tension Glaucoma
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 8 No. 4 (2019),
29 December 2019
,
Page 278-282
Abstract
Normal tension glaucoma (NTG) is a subtype of glaucoma that occurs at relatively low intraocular pressure levels and results in progressive optic neuropathy. Previous studies display some abnormal immune activity against the optic nerve. Neutrophil to lymphocyte (NLR) and platelet to lymphocyte ratios (PLR) are novel markers for inflammation. Here we evaluated the NLR, PLR, Creactive protein (CRP) and erythrocyte sedimentation rate (ESR) levels in NTG. NLR and PLR were resulted by dividing neutrophil and platelet counts to lymphocyte count respectively. Patients with a history of diabetes mellitus, chronic renal failure, rheumatologic disease, anemia, cancer, cigarette smoking, myocardial infarction and a febrile illness within one month of sampling were excluded from the investigation. In total, the blood samples of 28 NTG and 27control patients were analyzed for the study. There were 11 female (40.7%) and 16 male patients (59.3%) in the control group. The NTG group contained 15 (53.6%) female and 13 (46.4%) male patients. All of the NLR, PLR, ESR and CRP, values of NTG patients were not statistically different from the control group (P = 0.07, P = 0.64 and P = 0.44 respectively). Although previous studies have shown significant differences in NLR and PLR levels in other types of glaucoma, we did not find any significant difference in NTG subjects. Our early report may give insight into the differential diagnosis of NTG. Epub: October 1, 2019.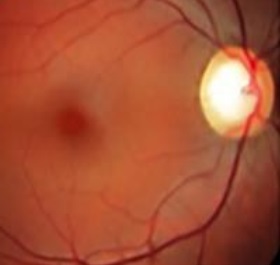
References
Shields MB. Normal-tension glaucoma: is it different from primary open-angle glaucoma? Curr Opin Ophthalmol. 2008;19(2):85-8. doi: 10.1097/ICU.0b01 3e3282f3919bpmid: 18301279
Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901-11. doi: 10.1001/jama.201 4.3192pmid: 24825645
Atalay K, Kaldirim Erdogan H, Kirgiz A, Asik Nacaroglu S. Predictive role of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in normal-tension glaucoma. Med Hypotheses. 2017;103:54-6. doi: 10.1016/j.mehy.2017.04.001pmid: 28571810
Meyer JH, Brandi-Dohrn J, Funk J. Twenty four hour blood pressure monitoring in normal tension glaucoma. Br J Ophthalmol. 1996;80(10):864-7. doi: 10.1136/bjo.80.10.864pmid: 8976695
Cartwright MJ, Grajewski AL, Friedberg ML, Anderson DR, Richards DW. Immune-related disease and normal-tension glaucoma. A case-control study. Arch Ophthalmol. 1992;110(4):500-2. doi: 10.1001/archoph t.1992.01080160078035pmid: 1562256
Yang J, Tezel G, Patil RV, Romano C, Wax MB. Serum autoantibody against glutathione S-transferase in patients with glaucoma. Invest Ophthalmol Vis Sci. 2001;42(6):1273-6. pmid: 11328739
Leibovitch I, Kurtz S, Kesler A, Feithliher N, Shemesh G, Sela BA. C-reactive protein levels in normal tension glaucoma. J Glaucoma. 2005;14(5):384-6. pmid: 16148587
Wax MB, Barrett DA, Pestronk A. Increased incidence of paraproteinemia and autoantibodies in patients with normal-pressure glaucoma. Am J Ophthalmol. 1994;117(5):561-8. doi: 10.1016/s0002-9394(14)700 59-5pmid: 8172259
Joachim SC, Pfeiffer N, Grus FH. Autoantibodies in patients with glaucoma: a comparison of IgG serum antibodies against retinal, optic nerve, and optic nerve head antigens. Graefes Arch Clin Exp Ophthalmol. 2005;243(8):817-23. doi: 10.1007/s00417-004-1094-5pmid: 15834611
Dong CH, Wang ZM, Chen SY. Neutrophil to lymphocyte ratio predict mortality and major adverse cardiac events in acute coronary syndrome: A systematic review and meta-analysis. Clin Biochem. 2018;52:131-6. doi: 10.1016/j.clinbiochem.2017.11.0 08pmid: 29132766
Uslu AU, Kucuk A, Sahin A, Ugan Y, Yilmaz R, Gungor T, et al. Two new inflammatory markers associated with Disease Activity Score-28 in patients with rheumatoid arthritis: neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Int J Rheum Dis. 2015;18(7):731-5. doi: 10.1111/1756-185X.12582pmid: 25900081
Rembach A, Watt AD, Wilson WJ, Rainey-Smith S, Ellis KA, Rowe CC, et al. An increased neutrophil-lymphocyte ratio in Alzheimer's disease is a function of age and is weakly correlated with neocortical amyloid accumulation. J Neuroimmunol. 2014;273(1-2):65-71. doi: 10.1016/j.jneuroim.2014.05.005pmid: 24907904
Ozgonul C, Sertoglu E, Mumcuoglu T, Kucukevcilioglu M. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Novel Biomarkers of Primary Open-Angle Glaucoma. J Glaucoma. 2016;25(10):e815-e20. doi: 10.1097/IJG.0000000000 000392pmid: 26918914
Ozgonul C, Sertoglu E, Mumcuoglu T, Ozge G, Gokce G. Prediction of Pseudoexfoliation Syndrome and Pseudoexfoliation Glaucoma by Using Neutrophil to Lymphocyte Ratio and Platelet to Lymphocyte Ratio. Ocul Immunol Inflamm. 2016;24(6):665-70. doi: 10.3109/09273948.2015.1063671pmid: 26645794
Sengul EA, Artunay O, Kockar A, Afacan C, Rasier R, Gun P, et al. Correlation of neutrophil/lymphocyte and platelet/lymphocyte ratio with visual acuity and macular thickness in age-related macular degeneration. Int J Ophthalmol. 2017;10(5):754-9. doi: 10.18240/ijo.2017.05.16pmid: 28546933
Dursun A, Ozturk S, Yucel H, Ozec AV, Dursun FG, Toker MI, et al. Association of neutrophil/lymphocyte ratio and retinal vein occlusion. Eur J Ophthalmol. 2015;25(4):343-6. doi: 10.5301/ejo.5000570pmid: 25633622
Sekeryapan B, Uzun F, Buyuktarakci S, Bulut A, Oner V. Neutrophil-to-Lymphocyte Ratio Increases in Patients With Dry Eye. Cornea. 2016;35(7):983-6. doi: 10.1097/ICO.0000000000000872pmid: 27158804
Celik T. Assessment of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Patients with Dry Eye Disease. Ocul Immunol Inflamm. 2018;26(8):1219-22. doi: 10.1080/09273948.2017.1340486pmid: 28910561
Ilhan C, Citirik M, Uzel MM, Tekin K. The Relationship of Neutrophil to Lymphocyte Ratio with Vitreomacular Traction Syndrome. Med Hypothesis Discov Innov Ophthalmol. 2019;8(1):22-7. pmid: 30923719
Mertoglu C, Gunay M. Neutrophil-Lymphocyte ratio and Platelet-Lymphocyte ratio as useful predictive markers of prediabetes and diabetes mellitus. Diabetes Metab Syndr. 2017;11 Suppl 1:S127-S31. doi: 10.1016/j.dsx.2016.12.021pmid: 28017281
Yaprak M, Turan MN, Dayanan R, Akin S, Degirmen E, Yildirim M, et al. Platelet-to-lymphocyte ratio predicts mortality better than neutrophil-to-lymphocyte ratio in hemodialysis patients. Int Urol Nephrol. 2016;48(8):1343-8. doi: 10.1007/s11255-016-1301-4pmid: 27118565
Chandrashekara S, Mukhtar Ahmad M, Renuka P, Anupama KR, Renuka K. Characterization of neutrophil-to-lymphocyte ratio as a measure of inflammation in rheumatoid arthritis. Int J Rheum Dis. 2017;20(10):1457-67. doi: 10.1111/1756-185X.13157pmid: 28952205
Iqbal T, Stein J, Sharma N, Kulnigg-Dabsch S, Vel S, Gasche C. Clinical significance of C-reactive protein levels in predicting responsiveness to iron therapy in patients with inflammatory bowel disease and iron deficiency anemia. Dig Dis Sci. 2015;60(5):1375-81. doi: 10.1007/s10620-014-3460-4pmid: 25501922
Templeton AJ, McNamara MG, Seruga B, Vera-Badillo FE, Aneja P, Ocana A, et al. Prognostic role of neutrophil-to-lymphocyte ratio in solid tumors: a systematic review and meta-analysis. J Natl Cancer Inst. 2014;106(6):dju124. doi: 10.1093/jnci/dju124pmid: 24875653
Kumari B, Aslam SK, Zaheer S, Adil SO, Shafique K. Systemic Inflammatory Markers Among Waterpipe Smokers, Cigarette Smokers, and Nonsmokers. J Addict Med. 2019;13(1):55-60. doi: 10.1097/ADM.0000000000000446pmid: 30063545
Cicek G, Acikgoz SK, Bozbay M, Altay S, Ugur M, Uluganyan M, et al. Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio combination can predict prognosis in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Angiology. 2015;66(5):441-7. doi: 10.1177/0003319714535970pmid: 24834932
Hodapp E, Parrish RK, Anderson DR. Clinical decisions in glaucoma: Mosby Inc; 1993.
Polat O, Yavas GF, Inan S, Inan UU. Neutrophil-to-Lymphocyte Ratio as a Marker in Patients with Non-arteritic Anterior Ischemic Optic Neuropathy. Balkan Med J. 2015;32(4):382-7. doi: 10.5152/balkanmedj.2 015.15689pmid: 26740898
Huang P, Qi Y, Xu YS, Liu J, Liao D, Zhang SS, et al. Serum cytokine alteration is associated with optic neuropathy in human primary open angle glaucoma. J Glaucoma. 2010;19(5):324-30. doi: 10.1097/IJG.0b013e3181b4 cac7pmid: 19730118
Altintas O, Yuksel N, Sonmez GT, Ozkan B, Altintas L, Caliskan S, et al. Serum antiphospholipid antibody levels in pseudoexfoliation. J Glaucoma. 2012;21(5):326-30. doi: 10.1097/IJG.0b013e318212 06cdpmid: 21423032
Su WW, Ho WJ, Cheng ST, Chang SH, Wu SC. Systemic high-sensitivity C-reactive protein levels in normal-tension glaucoma and primary open-angle glaucoma. J Glaucoma. 2007;16(3):320-3. doi: 10.1097/IJG.0b0 13e3180391a83pmid: 17438427
Malvitte L, Montange T, Vejux A, Baudouin C, Bron AM, Creuzot-Garcher C, et al. Measurement of inflammatory cytokines by multicytokine assay in tears of patients with glaucoma topically treated with chronic drugs. Br J Ophthalmol. 2007;91(1):29-32. doi: 10.1136/bjo.2006.101485pmid: 16943231
- Abstract Viewed: 1253 times
- Full Text PDF. Epub:Oct. 1, 2019 Downloaded: 547 times


